Gluten can increase gut permeability, trigger immune cross-reactivity with brain tissue, and release opioid-like peptides that affect mood and thinking. In this article, we’ll explore how gluten affects the brain, why you don’t need celiac disease to feel the effects, and how testing can provide real answers.
If you’re struggling with brain fog, anxiety, mood changes, or low energy, gluten might be the missing piece. Even without a celiac diagnosis, many people experience neurological symptoms tied to non-celiac gluten sensitivity—a condition that’s often overlooked.
For midlife women, these issues are frequently blamed on hormones or aging. But it’s worth asking: is your bagel or pasta silently affecting your brain? Gluten and brain health are closely connected through pathways involving the gut, immune system, and nervous system.
How Gluten Impacts Brain Health Through the Gut
Gluten can increase gut permeability—commonly known as “leaky gut.” When your intestinal lining is compromised, gluten fragments and byproducts like gluteomorphins can pass into the bloodstream (Fasano, 2009). These opioid-like peptides may influence mood, cognition, and behavior, contributing to gluten brain fog.
Gluten may also interfere with:
- Prodynorphin, a precursor to mood-regulating dynorphins, which may amplify anxiety or depression.
- Gut microbes, by feeding bacteria that influence cravings, mood, and neurotransmitter balance (Alcock et al., 2014).
Testing for Gluten Brain Fog: Gluteomorphins & Prodynorphin
Tests like the Wheat Zoomer or Cyrex Array 3X go beyond traditional celiac screening. They identify antibodies against gluteomorphins and prodynorphin—revealing if your body reacts to gluten’s brain-active compounds.
Benefits of testing include:
- Clarity on whether gluten brain fog or mood dips are real and measurable
- Personalized dietary guidance without guesswork
- Identification of early-stage immune reactivity before major symptoms arise
Even without celiac genes, you may still have gluten sensitivity—especially if stress, infections, or gut imbalance are in the mix (Tondolo et al., 2005).
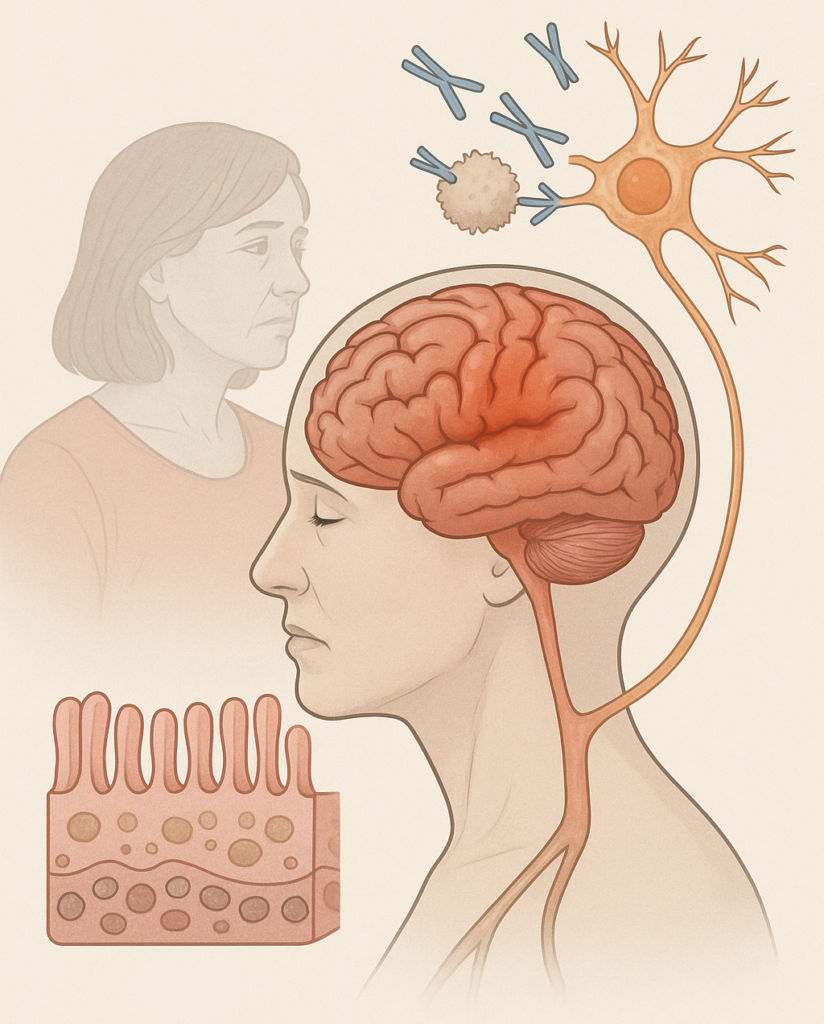
The Immune-Brain Connection
Gluten-related immune activity doesn’t stop at digestion. Antibodies formed against gluten fragments can cross-react with brain tissue due to molecular mimicry. This has been linked to:
- Autoimmune brain inflammation
- Neurological symptoms like ataxia, neuropathy, or cognitive decline
- Psychiatric conditions like schizophrenia and depression (Jackson et al., 2012)
Autoimmune disorders disproportionately affect women, especially during midlife hormonal shifts, making testing even more relevant.
Take Charge of Your Brain Health
Here’s how to take action if you suspect gluten may be affecting your brain:
- Consider Advanced Testing: Wheat Zoomer or Cyrex 3X can pinpoint reactions to gluten and brain-active peptides.
- Nourish Your Brain: Replace gluten-heavy foods with greens, sweet potatoes, salmon, and berries to reduce inflammation.
- Work with a Functional Medicine Expert: Get personalized guidance to interpret labs and design a realistic brain-friendly plan.
Real Results from Going Gluten-Free
Many people—especially those with neurological symptoms—report dramatic improvements from removing gluten and dairy (which also contains opioid-like compounds called casomorphins).
In one study, 80% of children with autism improved on a gluten- and casein-free diet (Cade et al., 2000). Adults with schizophrenia and depression have also shown benefit (Jackson et al., 2012).
While results vary, the science supports at least exploring this powerful connection.
Your Next Step
You deserve to feel sharp, energized, and emotionally balanced. If gluten is silently affecting your brain, the right testing and support can make all the difference.
Ready to investigate further? Start with the Wheat Zoomer or Neural Zoomer Plus to see if gluten-related antibodies are playing a role in your symptoms. I combine cutting-edge lab testing with personalized guidance to help you make informed, empowering choices—without feeling overwhelmed.
Choose your lab test:
- Order Wheat Zoomer
- Order Neural Zoomer Plus
- Order Neural Zoomer Plus w/ ApoE add-on
- Order Wheat Zoomer and Neural Zoomer Plus
👉 Click here to book a discovery call and begin your journey to better brain health.
References
- Alcock, J., Maley, C. C., & Aktipis, C. A. (2014). Is eating behavior manipulated by the gastrointestinal microbiota? BioEssays, 36(10), 940–949.
- Bressan, P., & Kramer, P. (2016). Bread and other edible agents of mental disease. Frontiers in Human Neuroscience, 10, 108.
- Cade, R., et al. (2000). Autism and schizophrenia: Intestinal disorders. Nutritional Neuroscience, 3(1), 57–72.
- Fasano, A. (2009). Surprises from celiac disease. Scientific American, 301(2), 54–61.
- Fasano, A. (2012). Zonulin, regulation of tight junctions, and autoimmune diseases. Ann NY Acad Sci, 1258(1), 25–33.
- Jackson, J. R., et al. (2012). Neurologic and psychiatric manifestations of celiac disease and gluten sensitivity. Psychiatric Quarterly, 83(1), 91–102.
- Sun, Z., & Cade, J. R. (1999). A peptide found in schizophrenia and autism causes behavioral changes in rats. Autism, 3(1), 85–95.
- Tondolo, V., et al. (2005). Genetics of celiac disease. Minerva Pediatrica, 57(6), 399–412.
+ show Comments
- Hide Comments
add a comment